India’s one of the world’s largest and most sophisticated healthcare systems is in the midst of a revolution, not only physician- and nurse-led but increasingly by an expanding and highly educated paramedical cadre as well. Paramedical personnel such as radiology technicians, laboratory technologists, physiotherapists, emergency medical technicians, and operation theatre attendants are the backbone of diagnostic, curative, and preventive medicine in both urban and rural India. Though the country is focusing on gaps in accessibility, affordability, and quality of care, the paramedical segment has a major role in transforming care delivery and contributing considerably to the sector’s performance and growth overall.
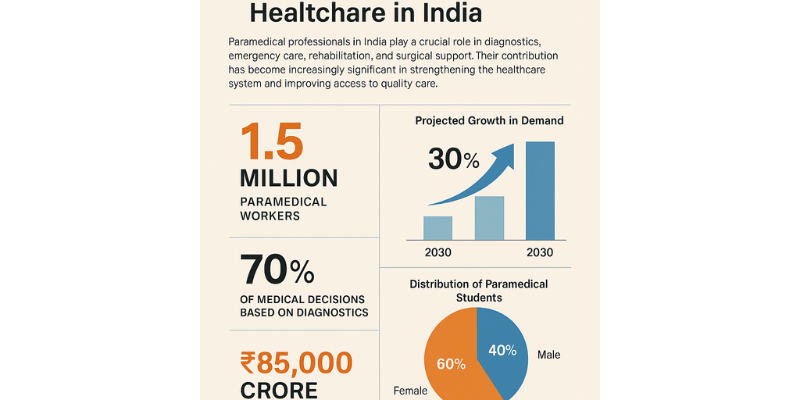
India’s healthcare sector was around USD 372 billion in 2022 and shall rise to USD 638 billion by the year 2030 and grow at a CAGR of about 8.5%. All this growth is the work of enabling areas such as diagnostics, rehabilitation, and emergency care—dominantly the work of paramedical professionals. India presently has more than 1.5 million paramedical professionals already, and demand should rise more than 30% by 2030 to cater to the demands of an increasing and aging population, rising disease burden, and additional emphasis placed on preventive and home care.
The most significant area where the paramedical sector makes its contribution is diagnostics which contributes to almost 70% of medical decisions. India’s diagnostics sector itself is more than ₹85,000 crore (USD 10 billion) in 2023, pathology and radiology combined. With more than 1.25 lakh diagnostic laboratories and more than 100,000 imaging facilities, lab technicians and radiographers who are trained remain the working support of this field. Machine and artificial intelligence-based diagnostic equipment still depend on properly trained human operators and experts, demonstrating the ongoing need for such operations. Introducing point-of-care diagnostic equipment to rural areas has also been able to enable paramedical staff to perform early and precise diagnoses of diseases such as tuberculosis, malaria, and diabetes.
Yet another most important area is emergency and trauma care, in which paramedics like ambulance attendants and emergency medical technicians (EMTs) are usually the first line of intervention. In the National Ambulance Services scheme, more than 26,000 ambulances have been rolled out all over India, meaning training and deployment of thousands of EMTs. These experts are of most use in stabilizing victims before arrival at hospitals and hence enhancing survival in accidents, cardiac arrests, and child birth emergencies. Tamil Nadu and Gujarat state governments have designed efficient pre-hospital emergency care systems with strict contact ratios of EMTs to patients, leading to a phenomenal reduction of trauma and health care emergencies in rural areas.
Physiotherapy and rehabilitation, especially post-operative, orthopedic, neurological, and geriatric, are increasingly essential. The incidence of non-communicable diseases (NCDs) such as diabetes, stroke, and cancer is increasing at a very rapid pace in India and contributes to over 60% of all deaths. Physiotherapists and occupational therapists are crucial in patients’ rehabilitation and quality of life. India needs over 600,000 physiotherapists, but there are only around 120,000 employed, with a enormous opportunity gap and demand.
India’s medical imaging and radiology services also quickly followed suit with the increasing trend of teleradiology and scans based on AI. Radiology technologists and imaging support staff are an invisible force that is keeping pace with the increasing number of CT, MRI, ultrasound, and X-ray machines in hospitals and diagnostic centers. As India operates more than 1.5 billion imaging scans every year, this industry alone is a large job generator. Moreover, the government’s focus on digital health, led by the likes of the Ayushman Bharat Digital Mission (ABDM), is empowering paramedics to effectively digitize patient records, aid remote diagnosis, and enhance coordination with healthcare professionals.
Operation theatre (OT) technicians, responsible for logistics, sterilization, and support in operating rooms, are required to. With an ever-increasing number of operations being conducted—running the gamut from cataract to orthopedic and cardiac operations—the need for OT technicians is also increasing. Multispecialty hospitals with large capacities typically employ 30–50 paramedical staff per 100 inpatient beds, indicative of the industry’s operational reliance on trained support staff.
The economic impact of the paramedical industry is massive. As per a report published by the National Skill Development Corporation (NSDC), there exists immense potential for paramedical training and services to generate over 5 million job opportunities in 2030 with an average annual income between ₹2–5 lakhs based on experience and specialization. In addition, skill development programs like the Skill India Mission, National Skill Development Programme, and Health Sector Skill Council (HSSC) are also encouraging curriculum standardization, accreditation improvement, and training infrastructure increases. More than 1.2 million candidates have undergone training under these initiatives for different healthcare positions since 2017 alone.
Involvement of women in the paramedical profession is also significant. With more than 60% of paramedical students being women, the profession is empowering women economically and socially, particularly from rural and semi-urban regions. Government and private sectors are promoting women-oriented paramedical courses with placement support and entrepreneurship skills training, especially in home healthcare services.
Technology is also expanding the role and effectiveness of paramedical personnel. Mobile health apps, teleconsultation websites, wearable diagnostic devices, and hand-held scanners have opened new avenues of paramedical services, particularly in rural and disadvantaged regions. Paramedics are also being trained in digital health literacy, electronic health record (EHR) management, and AI-based tools so they can provide faster and more accurate care to patients. Health-tech startups such as Practo, 1mg, and Portea heavily depend on paramedical professionals to grow their telemedicine and homecare businesses.
The COVID-19 pandemic placed the paramedical personnel under sharp scrutiny as being supremely pivotal. From carrying out mass screening, biomedical waste disposal, ICU backup, to vaccine delivery in remote health camps, paramedics were the caregiving frontline in moments when hospitals were stretched to their limits. Their resilience and operation in a state of crisis have prompted policymakers to revisit and revive policy attention on paramedical training and retention in the form of enhanced investment.
Challenges do still remain, however. Much as it is vital, India’s paramedical industry continues to grapple with low pay, insufficient standardization, poor regulation, and insufficient career options. Much remains unlicensed and untrained, and this produces uneven standards of care. Government bodies such as the Allied and Healthcare Professions Commission, created in 2021, are now attempting to deliver greater unity, licensing, and standardization to 50+ allied health professions.
At large, India’s paramedical industry is no longer a supporting pillar but a core element of healthcare revolution. Its growing presence—from diagnostics and emergency services to rehabilitation and surgery assistance—directly enhances the patient experience, system performance, and economic returns. With dedicated investment in training, certification, digital transformation, and employment-friendly practices, the paramedical industry can further propel India’s healthcare so that quality care becomes available to all at affordable cost.
Prepared by
Sureshkumar Mandala
Assistant Professor, School of CS&AI,
SR University, Warangal, Telangana 506371
m.suresh@sru.edu.in